Start Your Journey
Build Your Healthcare Venture the Right Way — Legally, Efficiently, and Hassle-Free
That’s where Lawfinity steps in — making the legal side of your healthcare business simple, fast, and future-proof.
INTRODUCTION
Healthcare in India is an important field that contributes to the country’s economy and society. It’s no longer just hospitals and doctors. It’s a sprawling edifice of services, technologies, diagnostics, equipment, digital platforms, and preventive care that provides more than a billion people with at least some modicum of health care. A tier-3 city clinic or a super-specialty hospital in Delhi, the demand for structured and organized licensed healthcare is being felt like never before.
In 2023, the value of India’s healthcare sector stood at above ₹23 lakh crore and is expected to cross ₹40 lakh crore by 2025. Boosted by increasing income levels, health consciousness, urbanization and Government schemes such as Ayushman Bharat and the National Digital Health Mission, the opportunity is massive. Start-ups, investors and medical professionals are clamouring to open up shop in healthcare—converting trucks into labs for diagnostic tests, rolling out diagnostic centers, opening new pharmacies or nursing homes or rehab centers, or even providing home care or telemedicine services.
But getting into health care isn’t a matter of capital and ambition alone. It’s a highly regulated space. Healthcare is a service business and its work changes and saves lives. A single mistake in complying can result in a shutdown, in penalties or even worse that may cost a human life. So, before you begin to invest anything in infrastructure or in hiring doctors, you must be very clear about what is the legal requirement for starting and running a healthcare business in India.
In this guide, we will take you through everything—from registering your company and the licences you require and state compliance, to how Lawfinity can assist with making the legal side of things easier.
TYPE OF BUSINESS SUITABLE FOR HEALTHCARE INDUSTRY
Choosing the right type of business structure is the first and arguably the most important step when entering the healthcare sector in India. Your business model, liability protection, funding ability and ease of getting approvals all depend on this one foundational choice.
- Sole Proprietorship or Partnership: Easy to start and low on cost, this structure is ideal for local clinics or single-pharmacy shops. However, it offers no personal liability protection, making it unsuitable for larger or risk-exposed healthcare ventures like hospitals or diagnostic labs.
- Limited Liability Partnership (LLP): LLPs offer limited liability and lower compliance, making them ideal for small-scale setups like dental clinics, labs, or rehab centers. However, they can’t raise equity or issue shares, limiting future scalability and investment opportunities.
- Private Limited Company (Pvt Ltd): The most preferred structure for hospitals, diagnostic chains, and health-tech startups. It offers liability protection, access to funding, and compliance readiness for licensing, empanelment, and government schemes. Ideal for scaling and long-term business sustainability in healthcare.
- Section 8 Company (Non-Profit): Perfect for charitable hospitals, public health NGOs, or free clinics. Operates as a non-profit entity, eligible for donations, CSR funds, and tax exemptions. Best suited for ventures focusing on healthcare accessibility, awareness, and community impact.
Which Structure is Best Suited? If you're starting a scalable, growth-oriented healthcare business—like a hospital, telemedicine platform, or diagnostic network—a Private Limited Company is the most suitable structure due to its legal protection, funding potential, and compliance compatibility. For charitable ventures, go with a Section 8 Company.
NECESSARY APPROVALS TO START A HEALTHCARE BUSINESS
Once your business structure is decided and registered, the next step is obtaining the statutory approvals necessary to build and operate your healthcare facility. These are mostly state-level clearances that must be obtained before you start clinical or commercial activities. Missing even one can result in show-cause notices or closure.
Let’s go over the major ones:
- Land Use and Building Plan Approval: Healthcare premises must be located in zones approved for medical use. Submit building plans, fire layouts, and zoning compliance to the municipal authority. Special permission is required for residential areas. Ensure rented properties align with healthcare usage norms.
- Consent to Establish & Operate (Pollution Control Board): Hospitals and clinics handling biomedical waste must obtain Consent to Establish (CTE) before construction and Consent to Operate (CTO) before launch from the State Pollution Control Board. This ensures responsible disposal and pollution control mechanisms are in place.
- Fire Safety NOC: A Fire Safety NOC from the local Fire Department is mandatory. It ensures fire exits, alarms, extinguishers, water tanks, and evacuation plans are installed. Without it, insurance claims may be denied, and operations can be legally halted.
- Clinical Establishment Registration: As per the Clinical Establishments Act, all clinics, hospitals, and labs must register with the District Health Authority. Details of services, staff, infrastructure, and patient care protocols are submitted. The license is mandatory and renewable every 1–3 years.
- Shops & Establishment Registration / Trade License: This registration, issued by the municipal authority, legally allows business operations and regulates work hours, hygiene, and employee conditions. In metro areas, a Trade License is also required for pharmacies, labs, or hospitals alongside healthcare-specific licences.
- AERB (Radiology Equipment) Approval: Facilities using X-Ray, CT, PET, or similar equipment must obtain approval from AERB. This ensures radiation safety, staff certification, lead shielding, and calibrated machinery. Legal operation of radiological devices is prohibited without AERB registration and compliance checks.
REQUIRED LICENSES FOR HEALTHCARE BUSINESSES IN INDIA
Approvals give you permission to build and operate, but licenses give you the legal authority to deliver specific services. These are issued under various central acts like the Drugs & Cosmetics Act, Biomedical Waste Rules, FSS Act and others. Based on your business model—clinic, hospital, pharmacy, lab or telehealth—you will need one or more of the following:
- Drug License (Retail & Wholesale): If your facility sells, stores, or dispenses medicine, a Retail or Wholesale Drug License is mandatory under the Drugs and Cosmetics Act, 1940. It requires a registered pharmacist, cold chain setup, inspection, and must be renewed regularly to avoid penalties.
- Biomedical Waste Management Authorization: Any healthcare unit generating biomedical waste—such as swabs, sharps, or fluids—must obtain authorization under the Biomedical Waste Management Rules, 2016. You must tie up with an approved CBWTF and submit annual disposal records to the State Pollution Control Board.
- PNDT (Pre-Conception and Pre-Natal Diagnostic Techniques) Registration: Ultrasound or fetal imaging centers must be registered under the PCPNDT Act, 1994. Machines must be declared, legal signage displayed, monthly reports submitted, and Form F maintained. Violations can result in sealing of the premises and cancellation of registration.
- FSSAI License: Hospitals or care centers with kitchens must obtain an FSSAI license to ensure food hygiene for patients. Requirements include clean facilities, pest control, food labeling, refrigeration, and periodic health checks of kitchen staff. Non-compliance invites inspections and financial penalties.
- Telemedicine Compliance: Teleconsultation services must adhere to the 2020 Telemedicine Guidelines. Only licensed doctors may consult online, with secure data handling, informed consent, and prescription restrictions. A standard operating procedure must be followed and audit logs maintained under the IT Act framework.
WHY APPROVALS AND LICENSES ARE NEEDED
Running a healthcare business in India without the necessary approvals and licenses is not just risky—it’s illegal. This industry deals directly with people’s health, safety and even life. That’s why the government has created strict compliance frameworks under various central and state laws to protect patients, regulate professionals and prevent unethical practices.
Let’s break down why these approvals and licenses aren’t just bureaucratic red tape, but essential tools for safe and responsible operations.
- To Ensure Public Health & Patient Safety: Licences ensure healthcare facilities meet safety norms. From qualified staff to clean environments, regulations like the Clinical Establishments Act and AERB standards prevent unethical practices, unsafe procedures, and patient harm. Without them, the risk to public health is severe.
- Legal Protection for Your Business: Operating without licences weakens your legal defense in malpractice claims and voids insurance coverage. Proper registrations prove regulatory compliance and responsible business conduct—crucial when facing patient lawsuits, audits, or disputes in court or consumer forums.
- Regulatory Trust & Eligibility for Empanelment: Valid licences are mandatory for empanelment under government health schemes and private insurers. Without Pollution NOC, Fire NOC, or FSSAI, you're ineligible for tenders or contracts—blocking access to major revenue channels and long-term institutional partnerships.
- Avoiding Penalties and Shutdowns: Non-compliance invites heavy fines, license cancellations, and even criminal prosecution. States actively seal unregistered clinics and penalize violations like illegal ultrasounds or unhygienic kitchens. Once shut down, re-approvals are time-consuming—disrupting patient care and damaging your brand’s reputation.
HOW LAWFINTIY CAN HELP YOU ESTABLISH YOUR HEALTHCARE BUSINESS
At Lawfinity, we understand how overwhelming it can be to deal with government departments, confusing regulations, inspections and document requirements. That’s why we offer end-to-end legal and compliance services tailored specifically for India’s healthcare sector.
Whether you are a first-time entrepreneur, a team of doctors starting a multi-specialty hospital or a startup founder building a telemedicine platform, we step in as your legal backbone—so you can focus on building and serving patients, while we handle the paperwork, coordination and follow-ups.
Here’s how we help:
i. Company Registration & Structuring
We help you choose the right structure—Private Limited, LLP or Section 8 Company—and register it with the Ministry of Corporate Affairs. We also assist in getting your PAN, TAN, GST, MSME and opening a current account. If you are expanding or restructuring, we also handle share transfers, equity dilution or investor onboarding.
ii. Licenses & Registrations
We manage the entire licensing workflow:
- Clinical Establishment Registration
- Retail/Wholesale Drug License
- Biomedical Waste Authorization
- FSSAI license
- Fire NOC
- Trade/Shop Act Registration
- PNDT Act compliance
- AERB Registration for radiology setups
- Pollution NOCs (CTE and CTO)
We don’t just fill forms. We guide you on the right categories, draft SOPs, prepare affidavits and upload compliance documentation on official portals. Our team knows how to navigate state-specific requirements in Delhi, Maharashtra, Karnataka, UP, Haryana, Gujarat and others.
iii. Compliance Management
Getting a license is only step one. Renewing it on time, maintaining registers, preparing for inspections—that’s the real game. Lawfinity offers renewal tracking, yearly reporting assistance and audit prep to keep your business legally safe throughout the year.
iv. Drafting & Documentation
We also handle legal documentation such as:
- Lease agreements for clinics or hospitals
- Doctor and staff contracts
- Standard Operating Procedures (SOPs) for waste handling
- Telemedicine Terms of Use
- Vendor & lab tie-up agreements
- Nursing home bylaws
v. Telemedicine & Startup Support
If you are a digital health startup, we help with:
- Platform legal compliance (Telemedicine Guidelines 2020)
- Doctor verification & consent workflows
- Data privacy terms
- Legal disclaimers and app documentation
Need help launching your healthcare business legally?
Visit www.lawfinity.in or contact our legal team today. Whether you are a hospital chain, diagnostic lab or digital health founder—we are with you from Day 1 to Year 10.
INDIAN HEALTHCARE INDUSTRY REVENUE (2014–2024)
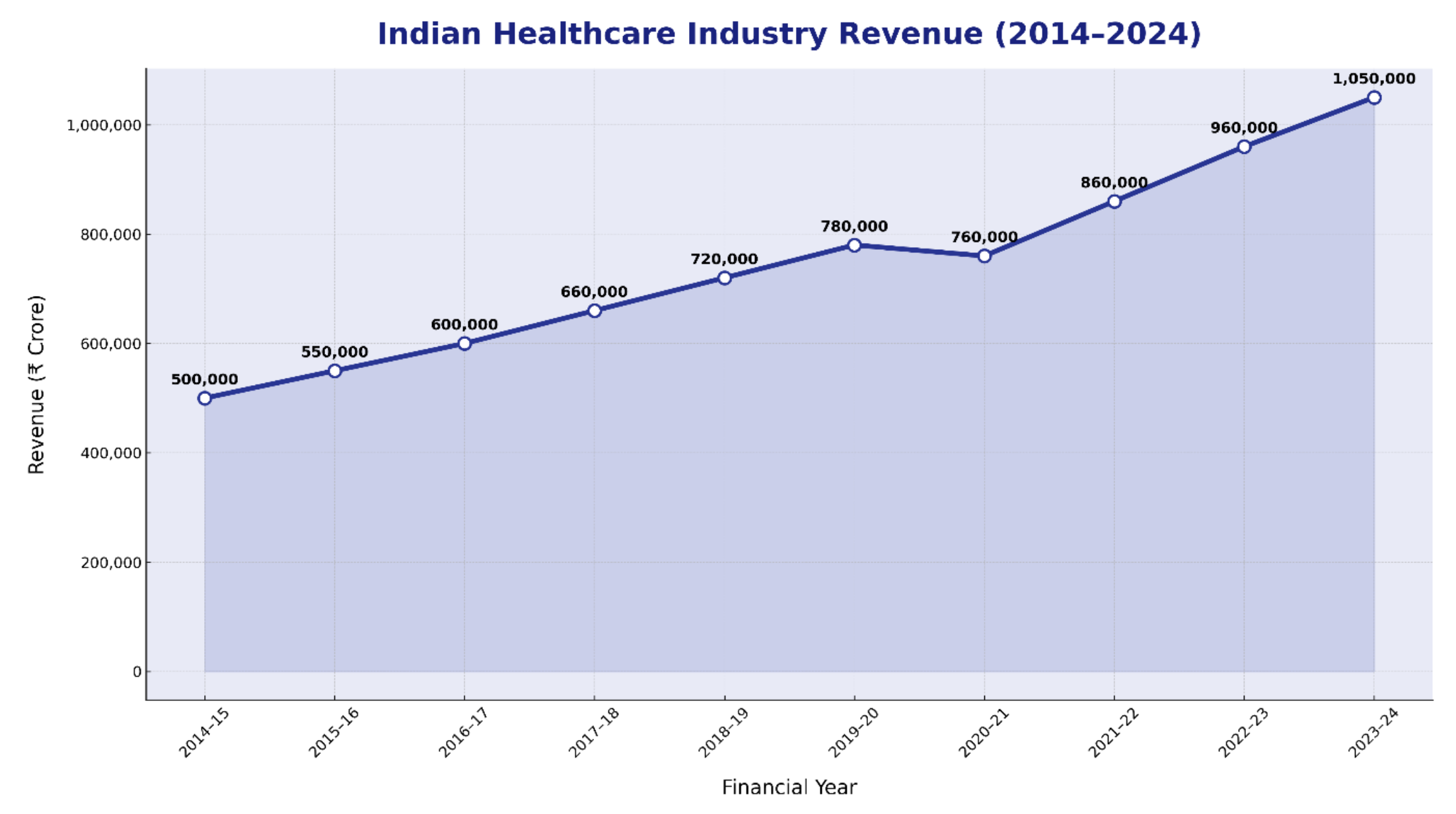
Source: India Brand Equity Foundation (IBEF) – Healthcare Reports 2020–2023, FICCI & EY Healthcare Reports (2021–2023), CRISIL & PwC India Healthcare Outlooks and MoHFW & NITI Aayog Sectoral Reports
This graph captures the revenue growth of the Indian Healthcare Industry over the last ten financial years, from FY 2014–15 to FY 2023–24, shown in INR crore.
- In FY 2014–15, the industry was valued at approximately ₹5,00,000 crore.
- The sector steadily expanded year after year, reaching ₹7,80,000 crore by FY 2019–20.
- A minor contraction in FY 2020–21 due to COVID-19 disruptions saw revenue dip to ₹7,60,000 crore.
- Post-pandemic recovery and structural transformation pushed the industry to ₹10,50,000 crore in FY 2023–24 — the highest ever in India’s healthcare sector history.
AUTHOR’S OPINION: A DECADE OF HEALING, INNOVATION & GROWTH
The Past: Fragmented Yet Rapidly Expanding
Ten years ago, India’s healthcare sector was undergoing quiet but steady expansion. Revenue stood at about ₹5 lakh crore in FY 2014–15, largely driven by private hospitals, traditional pharma companies and pathology labs. The industry was fragmented — with uneven urban–rural distribution, inconsistent infrastructure and over-dependence on out-of-pocket spending.
Still, increased insurance penetration, rising awareness and private sector investment kept the sector growing. Between FY 2014–15 and FY 2019–20, the industry nearly doubled in size. Private hospital chains like Apollo, Fortis and Max expanded aggressively, while health-tech startups began to emerge. Government schemes like Ayushman Bharat and the National Health Mission added scale to public healthcare delivery.
By FY 2019–20, the sector had reached an estimated ₹7.8 lakh crore, reflecting the combined strength of hospitals, diagnostics, medical tourism and retail pharma.
The Present: Post-Pandemic Acceleration & Structural Reform
The sudden outbreak of COVID-19 in 2020–21 disrupted routine healthcare services across the country. Elective surgeries were postponed, OPDs were shut and diagnostics declined, causing a temporary dip in revenue to ₹7.6 lakh crore. However, the crisis also brought about a massive shift in health system priorities — transforming India’s healthcare from reactive to proactive.
From FY 2021–22 onward, healthcare saw a strong resurgence, bolstered by telemedicine, e-pharmacies, homecare and public-private vaccine delivery models. Digital health infrastructure like ABHA (Ayushman Bharat Health Account) and the National Digital Health Mission gained traction. Investors poured capital into health-tech platforms, while Tier-II cities witnessed hospital expansion.
By FY 2023–24, the sector’s revenue climbed to a record ₹10.5 lakh crore, reflecting not just growth in volume, but maturity in service delivery, regulation and innovation. Healthcare is now viewed not just as a service, but as an essential pillar of national security and economic resilience.
The Future: Tech-Enabled, Equitable and Investment-Friendly
Looking ahead, India’s healthcare industry is poised for exponential growth. With a projected CAGR of 12%–15%, the sector is expected to cross ₹18–20 lakh crore by 2030. Growth will be driven by multiple factors:
- Digitization: Expansion of telemedicine, AI diagnostics and electronic health records.
- Affordability: Rising demand for low-cost insurance and subscription-based care models.
- Infrastructure: Development of medical colleges, hospitals and diagnostic labs in under-served regions.
- Policy Focus: Continued government investment in preventive healthcare, digital platforms and universal coverage.
- Foreign Investment: FDI-friendly regulations and rising interest from global healthcare investors.
Yet, challenges remain — shortage of skilled professionals, uneven quality standards and an urban-rural care gap. For the sector to realize its full potential, reforms must be accompanied by on-ground implementation, data-driven governance and better last-mile delivery.
CONCLUSION: AN INDUSTRY TRANSFORMED BY CRISIS AND INNOVATION
From my perspective, the last ten years have reshaped India’s healthcare industry more than any decade before. What began as a fragmented, metro-focused market has evolved into a nationwide health ecosystem — with private innovation, public policy and digital acceleration coming together.
The Indian healthcare industry is no longer just a service sector — it is now an engine of national resilience, economic value and social justice.
With sustained investment, equitable policy design and tech-led delivery models, the next decade will not just be about treating illness — it will be about creating accessible, accountable and anticipatory healthcare for all Indians.
Frequently Asked Questions
Because every great business starts with the right answers.
Yes. Every medical practice—regardless of size or number of staff—must register under the Clinical Establishments Act if your state has adopted it.
No. A qualified pathologist is mandatory to supervise lab operations and sign off on reports. Hiring a part-time pathologist is acceptable but must be declared.
Your platform must follow Telemedicine Guidelines, employ registered doctors, maintain data privacy and operate under a legally incorporated entity.
Typically 20–45 days, depending on inspection availability and document accuracy. Some states now offer online tracking through the SUGAM portal.
Yes. If you use ultrasound for any prenatal diagnosis, you must register under the PNDT Act and follow its strict reporting guidelines—even if you are fully compliant.
Operating without it is illegal. You could face penalties, environmental violation notices and even closure by the State Pollution Board.
Yes. We have handled cases across India—from metros to small towns. Our team understands local authority processes and can guide you with documentation and liaison.
Yes. If food is prepared or served on your premises (whether free or paid), you need FSSAI registration or license.
Core medical services are GST-exempt, but diagnostic labs, cosmetic procedures and telehealth may need registration if turnover exceeds ₹20–40 lakh depending on state.